On June 4, the Department of Health and Human Services (HHS) announced that it expanded Certified Community Behavioral Health Clinic (CCBHC) Medicaid funding for ten additional states, increasing access to mental health and substance use services for people who need it most. Learn more about the CCBHC model, the expansion of the CCBHC Medicaid Demonstration program and how Genoa Healthcare® pharmacy services can help you get the most out of your CCBHC status.
What is a CCBHC?
A CCBHC is a clinic that offers a range of mental health and substance use services to people seeking care – regardless of their diagnosis or ability to pay. Serving an estimated 3 million people per year, CCBHCs are responsible for delivering nine specific services to their consumers, including outpatient mental health and substance use services, crisis services and outpatient primary care screening and monitoring. They’re also required to meet specific criteria, like care coordination, service accessibility and reporting measures. CCBHCs receive flexible funding to support the costs of providing these expanded services that meet the needs of their communities.
How are CCBHCs funded?
CCBHCs are funded through Substance Abuse and Mental Health Services (SAMHSA) grants or the CCBHC Medicaid Demonstration program. As a part of the CCBHC program, most CCBHCs are reimbursed through the Prospective Payment System 1, a fixed daily rate that averages $245 per day. Other CCBHCs are funded through the Prospective Payment System 2, which reimburses CCBHCs through a fixed, monthly rate per beneficiary and averages $710 per month. The remaining clinics operate on a fee-for-service basis, which varies state by state and is set by State Medicaid agencies. Performance reporting is required for reimbursement regardless of which reimbursement payment model a CCBHC uses.
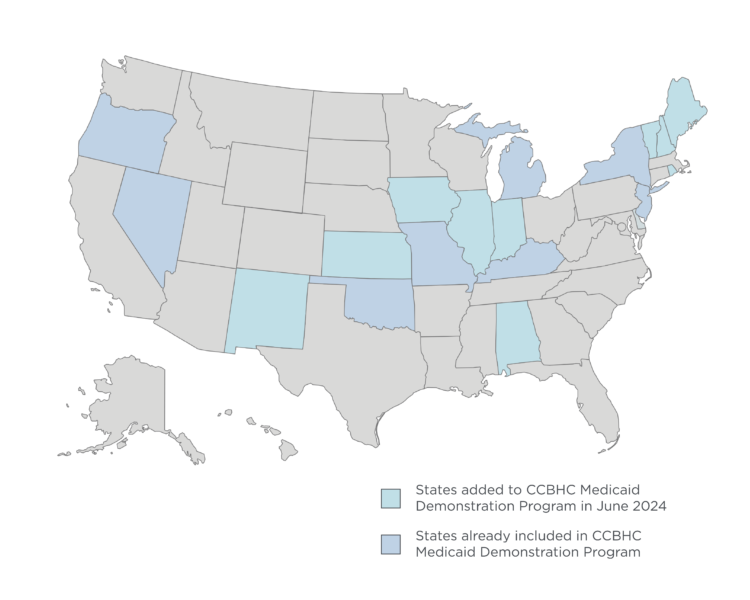
What states are eligible for newly expanded CCBHC Medicaid funding?
The recently signed Bipartisan Safer Communities Act authorizes HHS to add 10 states to the CCBHC Medicaid Demonstration program every two years. On June 4, HHS announced that CCBHCs in Alabama, Illinois, Indiana, Iowa, Kansas, Maine, New Hampshire, New Mexico, Rhode Island and Vermont could begin receiving reimbursement through Medicaid. These states join eight others in the CCBHC Medicaid Demonstration program, including Michigan, Missouri, Kentucky, Nevada, New Jersey, New York, Oklahoma, and Oregon.
How can a pharmacy, like Genoa, support my CCBHC?
Whether your clinic is a current CCBHC or is thinking about getting certified, a pharmacy can help ensure you get the most out of the CCBHC program. Genoa, a behavioral health pharmacy, works closely with over 200 CCBHCs across the U.S., supporting their efforts to demonstrate criteria for maintaining CCBHC status and submitting grant proposals.
Genoa’s personalized, high-touch pharmacy services can help your CCBHC increase the accessibility of services and services offered, care coordination and data and reporting, including medication adherence and other outcomes. Beyond that, Genoa can help you develop your CCBHC grant requests to ensure they include the correct pharmacy data and information.
Let’s connect
Want to learn more about how Genoa can help your clinic get the most out of the CCBHC program? Fill out the form below and we’ll be in touch.
"*" indicates required fields
About the author
As Director of Partnerships & Client Success, LaTonage Porter, RPh, FASCP, FAB, is responsible for helping Genoa Healthcare retain and grow its partnerships with behavioral health and other specialty clinics across the U.S. Before her current role, Porter served as Divisional Vice President, overseeing the operation of Genoa’s pharmacies in the Midwest and Director of Operations for its pharmacies in Texas, Alabama, Mississippi and Louisiana. Porter received her Bachelor of Science and Pharmacy from Auburn University Harrison College of Pharmacy in 1999.





